SurgiPrint ®
Leading the edge of Surgical AI
The WHY ? 4 majors beneficiaries
A Win - Win - Win -Win Relationship!
For Practitioners👨⚕️🔬
AI-powered 3D models provide surgeons with precise, patient-specific anatomical insights, enhancing pre-operative planning, reducing uncertainties, and improving surgical outcomes—all in a fraction of the time.
For Patients🏥💙
Personalized 3D visualizations help patients understand their condition better, leading to informed decision-making, fewer complications, and faster recoveries with optimized, minimally invasive procedures.
For Hospitals & Clinics🏥📉
AI-driven 3D modeling enhances surgical precision, reducing operation times and post-op complications. This leads to optimized resource use, fewer ICU admissions, and shorter hospital stays—ultimately improving efficiency and patient throughput.
For Healthcare Insurers💰✅
Fewer complications and optimized surgical planning translate into lower healthcare costs. Reduced hospital stays, fewer re-interventions, and improved patient outcomes mean significant savings while maintaining high-quality care standards.
The HOW ? 3 EASY STEPS
From DICOM to deep AI analysis

1. DRAG AND DROP
DICOM - CT Scans, PET Scans, MRI Medical images are uploaded to our secured server in seconds.

2. SurgiPrint AI Analysis
Our AI algorithm, along with our team of dedicated radiologists will process the DICOM
3. Easy link access
SurgiPrint will provide a link with the complete analysis - which is immediately accessible on any device just by a click. No requirement of any software installation.
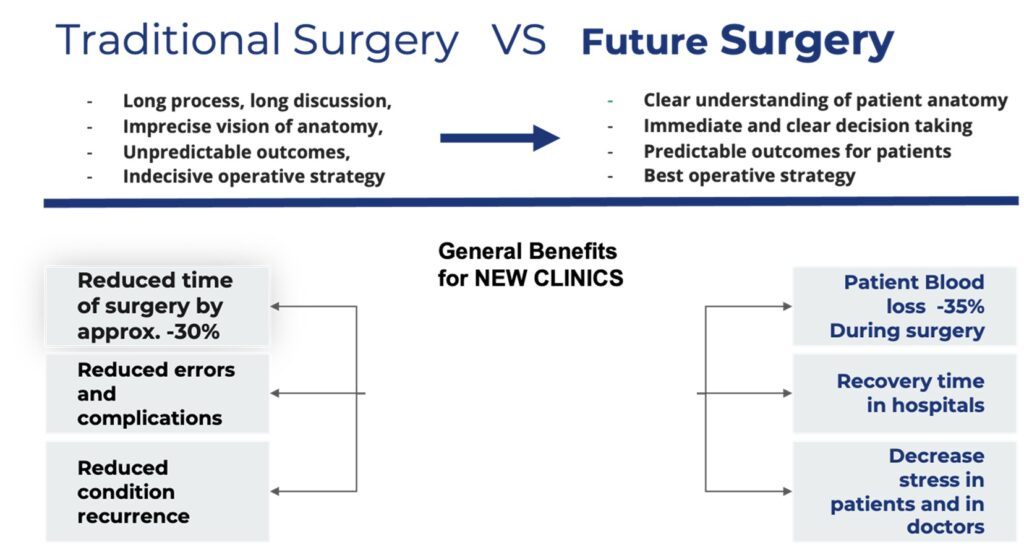
Surgical planning Benefits Explained
🚀 Revolutionizing Medical Imaging with 3D Model Reconstruction 🚀
In today’s rapidly evolving medical field, the leap from traditional 2D CT scans and MRIs to dynamic 3D model reconstructions marks a monumental shift in patient care and surgical precision. 🏥💡
Why is this transition so pivotal? Let’s dive in:
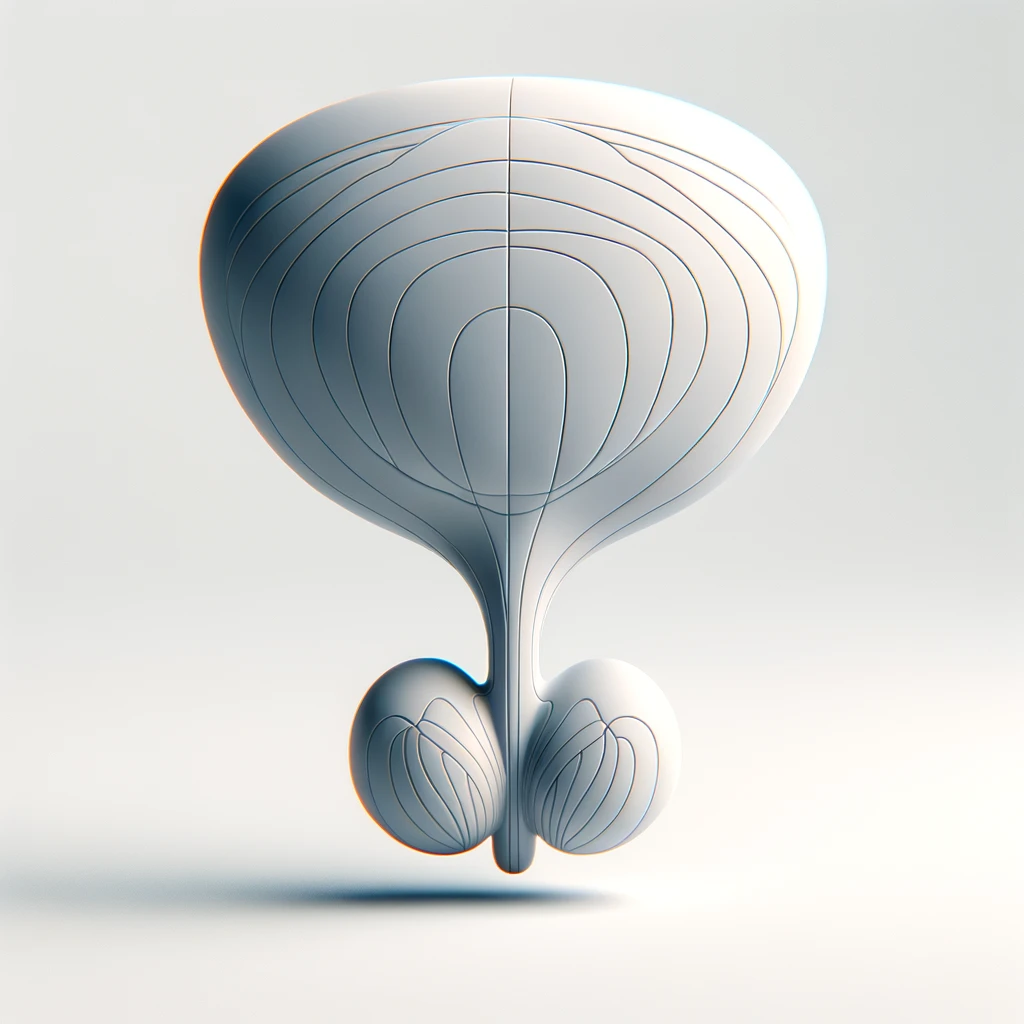
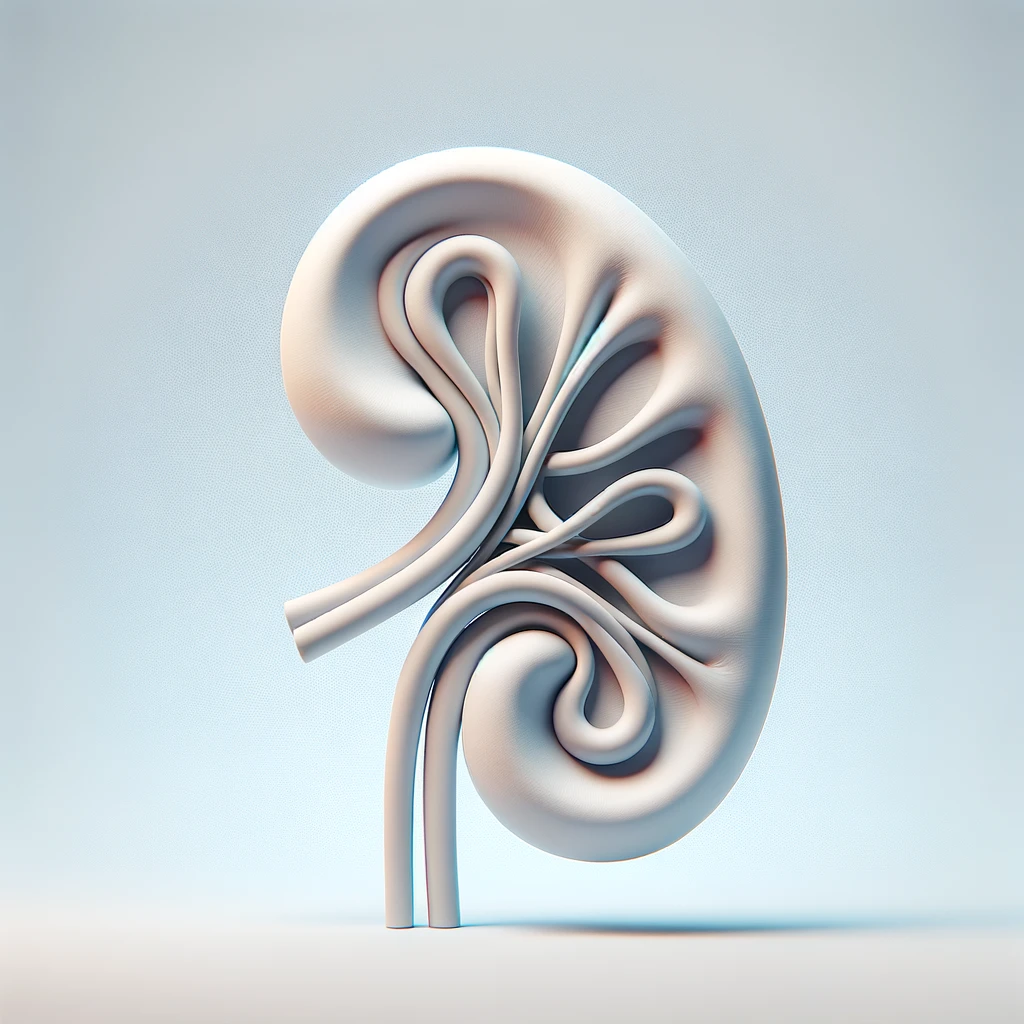
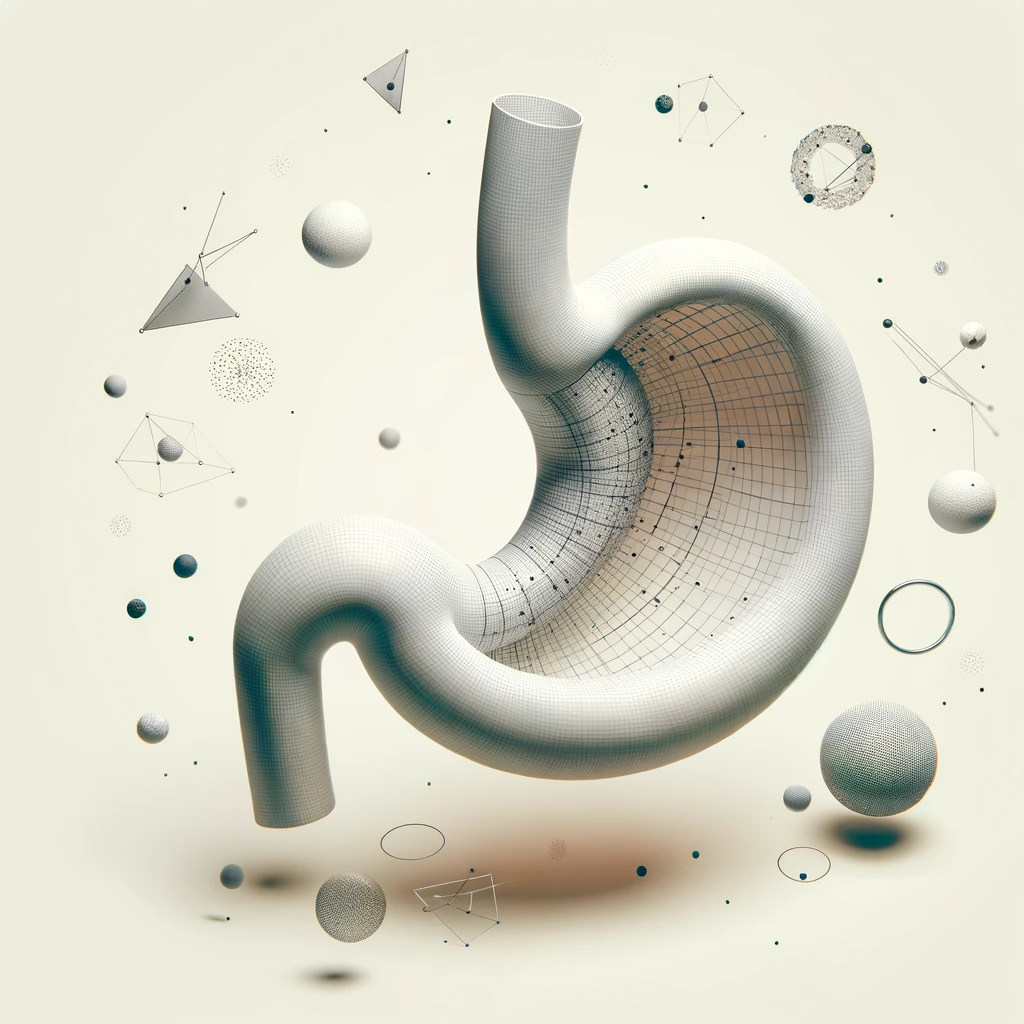
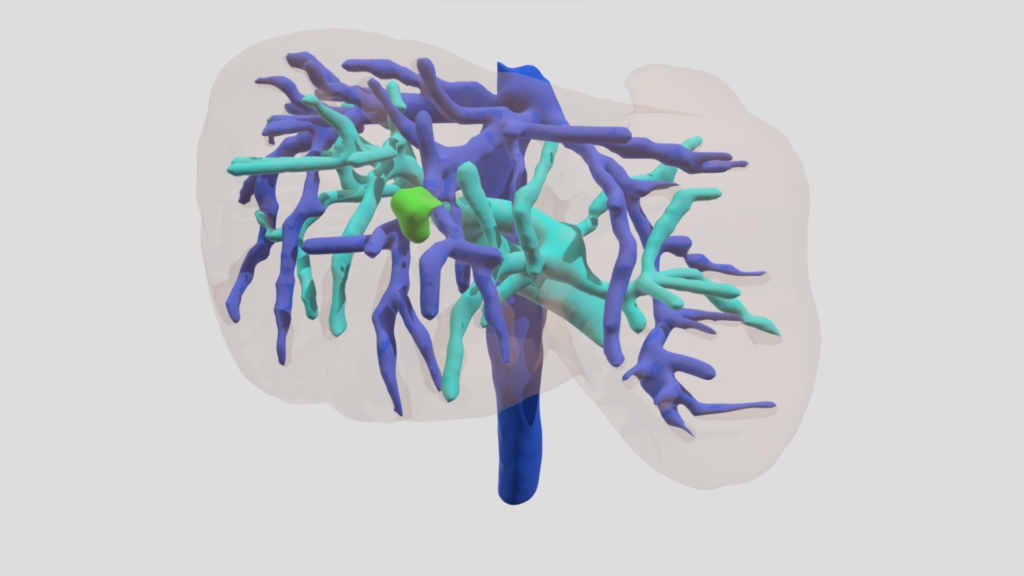
Enhanced Visualization 🌈: 3D models provide an unprecedented view of the human body’s intricate structures, allowing doctors and surgeons to navigate and understand complex anatomies with greater depth and clarity.
Precision Planning 🔍: Pre-surgical planning has never been more accurate. With 3D reconstructions, surgeons can strategize procedures with pinpoint accuracy, reducing uncertainties and improving outcomes.
Customized Patient Care 👤: Every patient is unique, and 3D modeling embraces this, offering tailored visualizations based on individual scans. This personalized approach ensures better preparation and patient-specific treatment strategies.
Educational Excellence 📚: For medical students and professionals alike, 3D models serve as powerful educational tools, enhancing learning and training experiences by providing hands-on, interactive studies of human anatomy and surgical techniques.
Innovative Solutions 🌟: The field of medical research and device development benefits greatly from 3D models, paving the way for the design of cutting-edge medical devices and therapeutic techniques.
In conclusion, the shift to 3D model reconstruction from traditional imaging methods is not just a technological upgrade; it’s a paradigm shift in medical diagnostics, treatment planning, and education. The future of healthcare is here, and it’s three-dimensional. 🌍🔬
Patient Education
Having the surgery explained well to a patient comfort his trust in both the doctor and the surgical operation. 3D reconstructed anatomy models are proving invaluable in facilitating patient understanding of prospective surgeries and procedures.
Pre-Op
The surgeon will have a significantly improved understanding of the work he has to do. Surgeons can now gain the benefit of an unobstructed 3D patient-specific view of hidden tissues and blood vessels.
During Op
Studies show the 3 following improvements : duration of surgical operations is decreased significantly ; as well as the average volume of bleeding ; drastic increase of the number of lymph node dissections.
Post-Op
The overall outcome of the surgery prove to have much improved results by the following metrics : Decrease of the Postoperative flatus recovery time ; Decrease of the Duration of hospitalization. The studies show a general satisfaction rate improvement for both the patient and the doctor of over 30%.